AI-based differential diagnosis of dementia etiologies on multimodal data
Jul 4, 2024·,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,,·
0 min read
Chonghua Xue*
Sahana S. Kowshik*
Diala Lteif
Shreyas Puducheri
Varuna H. Jasodanand
Olivia T. Zhou
Anika S. Walia
Osman B. Guney
J. Diana Zhang
Serena T. Pham
Artem Kaliaev
V. Carlota Andreu-Arasa
Brigid C. Dwyer
Chad W. Farris
Honglin Hao
Sachin Kedar
Asim Z. Mian
Daniel L. Murman
Sarah A. O’Shea
Aaron B. Paul
Saurabh Rohatgi
Marie-Helene Saint-Hilaire
Emmett A. Sartor
Bindu N. Setty
Juan E. Small
Arun Swaminathan
Olga Taraschenko
Jing Yuan
Yan Zhou
Shuhan Zhu
Cody Karjadi
Ting Fang Alvin Ang
Sarah A. Bargal
Bryan A. Plummer
Kathleen L. Poston
Meysam Ahangaran
Rhoda Au
Vijaya B. Kolachalama
Abstract
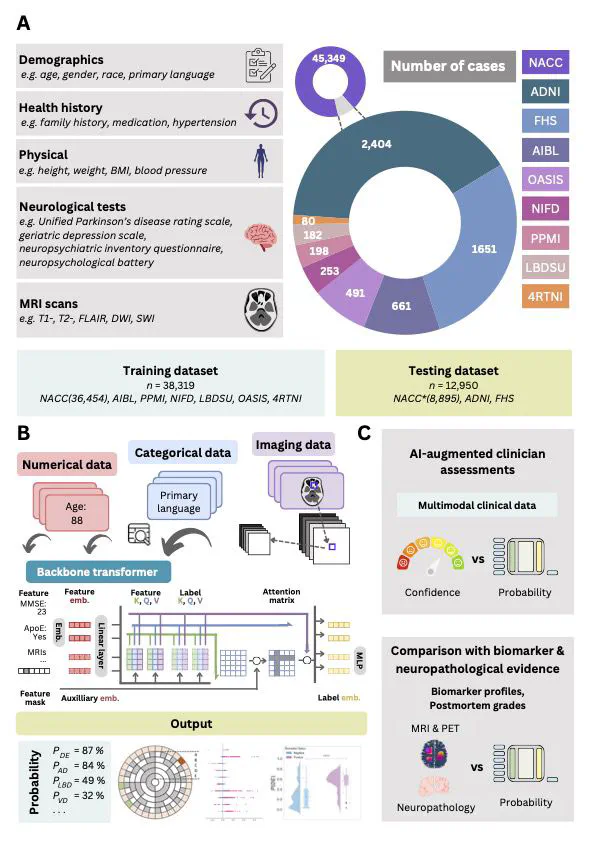
Differential diagnosis of dementia remains a challenge in neurology due to symptom overlap across etiologies, yet it is crucial for formulating early, personalized management strategies. Here, we present an artificial intelligence (AI) model that harnesses a broad array of data, including demographics, individual and family medical history, medication use, neuropsychological assessments, functional evaluations and multimodal neuroimaging, to identify the etiologies contributing to dementia in individuals. The study, drawing on 51,269 participants across 9 independent, geographically diverse datasets, facilitated the identification of 10 distinct dementia etiologies. It aligns diagnoses with similar management strategies, ensuring robust predictions even with incomplete data. Our model achieved a microaveraged area under the receiver operating characteristic curve (AUROC) of 0.94 in classifying individuals with normal cognition, mild cognitive impairment and dementia. Also, the microaveraged AUROC was 0.96 in differentiating the dementia etiologies. Our model demonstrated proficiency in addressing mixed dementia cases, with a mean AUROC of 0.78 for two co-occurring pathologies. In a randomly selected subset of 100 cases, the AUROC of neurologist assessments augmented by our AI model exceeded neurologist-only evaluations by 26.25%. Furthermore, our model predictions aligned with biomarker evidence and its associations with different proteinopathies were substantiated through postmortem findings. Our framework has the potential to be integrated as a screening tool for dementia in clinical settings and drug trials. Further prospective studies are needed to confirm its ability to improve patient care.
Type
Publication
Nature Medicine